01 Nov Your Feet and Diabetes – What You Should Know
Written By: Leslye Wolf, Director of Clinical Management
Type 2, adult onset, diabetes is the most common form of diabetes and is the result of your body not using its available insulin properly. Some people can control their diabetes with diet modifications and healthy eating but other may need to take medication or insulin daily. In 2021 it has been estimated that 38.1 million people in the US over the age of 18 years old had diabetes and for those over the age of 65 years of age 29.2% of this population had diabetes.
Diabetes can effect the body is several ways. A few of these effects can include high blood sugar levels which can thicken the blood and impact vision. This can lead to blurred vision or permanent vision loss. Diabetes can reduce the kidneys’ ability to filter waste, which can lead to chronic kidney disease. Diabetes can damage nerves in the body, which can cause pain, tingling, burning, and loss of feeling. Nerve damage in the feet, along with sores and infections, can lead to foot ulcers and may lead to amputation if not treated.
the diabetic foot
Excess blood sugar levels can decrease the elasticity of the small blood vessels which can cause them to narrow and restrict blood flow. When blood vessels aren’t working properly, blood that carries oxygen and nutrients can’t reach the parts of the body it needs to. This can include the skin and nerves and may lead to irreversible nerve damage, loss of feeling, and delayed healing in parts of the body. The result of this nerve damage is called peripheral neuropathy and you may notice several symptoms including:
- Tingling or numbness
- Burning pain
- Paralysis
- Muscle weakness
- Cramps
- Muscle twitching
- Loss of muscle and bone
- Changes in skin, hair, or nails
- Loss of balance
These are all a result of nerve damage. But the numbness can be the most damaging. Pain is a signal in your nervous system that something may be wrong in the body. And with peripheral neuropathy the pain signals may never reach the brain. This is why it’s very important to take preventative steps.
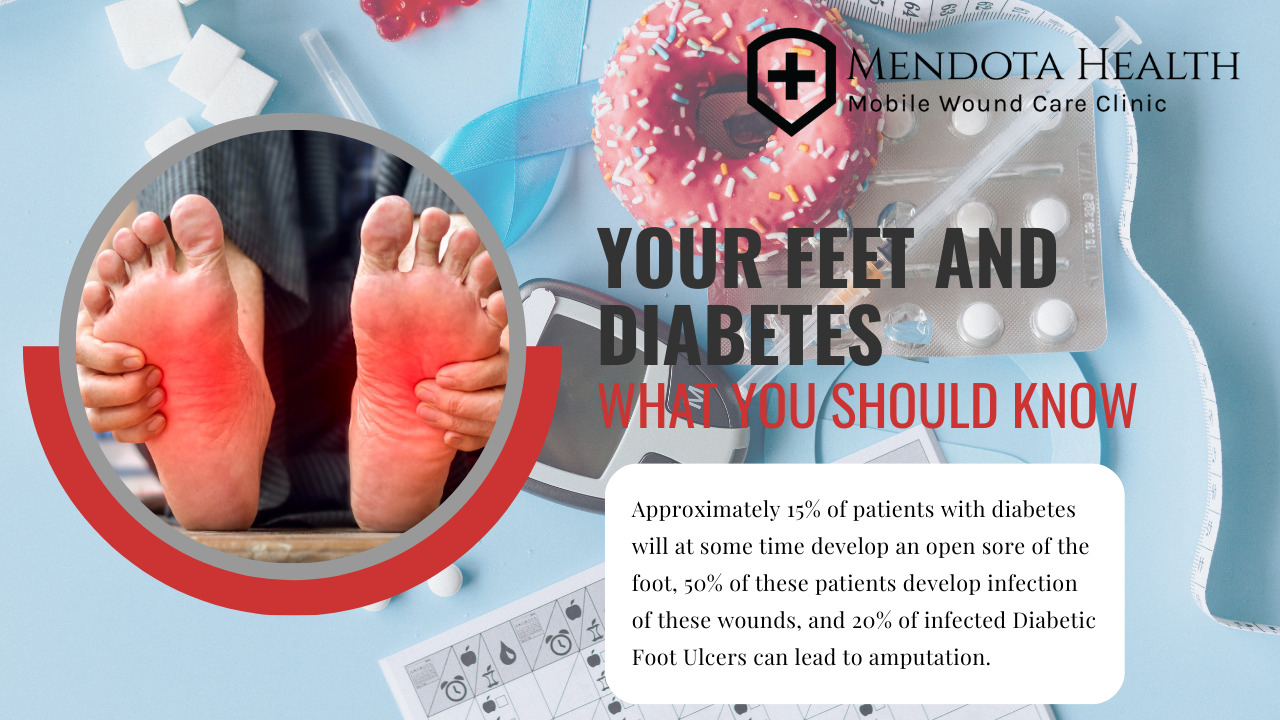
Aproximately 15% of patients with diabetes will at some time develop an open sore of the foot, 50% of these patients develop infection of these wounds, and 20% of infected DFUs can lead to amputation.
diabetic foot wounds
These are also known as diabetic foot ulcers (DFUs) and are open sores which develop on the feet of those with diabetes. These wounds are usually caused by a combination of peripheral neuropathy, peripheral arterial disease (PAD), and trauma/injury. The neuropathy causes a loss of sensation in the feet. PAD affects the blood flow to the feet due to damage to the walls of your arteries and abnormalities in your blood cells. Trauma/injury can be caused by simply stubbing a toe or wearing ill-fitting shoes, but this trauma often goes unnoticed since the pain sensors are damaged.
DFUs can become infected and may result in osteomyelitis, an infection of the bone, which can lead to amputation. Approximately 15% of patients with diabetes will at some time develop an open sore of the foot, 50% of these patients develop infection of these wounds, and 20% of infected DFUs can lead to amputation. This is why it is very important to take care of your feet if you have diabetes.
so what can you do?
Check your feet every day for cuts, redness, swelling, sores, blisters, corns, calluses, or other change to the skin or nails. If you cannot see the bottom of your feet then use a mirror to do so or ask a family member to help.
Wash your feet every day in warm (not hot) water. Don’t soak your feet in water. Be sure you dry your feet completely and apply a lotion to the tops and bottoms of your feet. Carefully dry between your toes and do not use lotion between them.
Never go barefoot. To prevent injury to your feet, always wear shoes and socks or slippers, even when you are inside. Check the inside of your shoes before you put them on to be sure that there aren’t any pebbles or other foreign objects in them. Make sure that the lining, if any, is smooth without wrinkles or puckers.
Wear shoes that fit well. Wear your diabetic shoes if prescribed by your doctor. Always wear socks with your shoes to prevent them from rubbing against your feet. If you purchase new shoes, break them in slowly by wearing them for an hour or two a day until they’re completely comfortable.

Trim your toenails straight across and gently smooth any sharp edges with a nail file. If you can’t see or reach your feet have your foot doctor, podiatrist, trim your toenails.
Don’t remove corns or calluses yourself. Let your podiatrist do this. Over the counter corn and callous removal creams can contain substances that can burn your skin. If you have neuropathy you may not feel the pain associated with this damage. It is advised not to use these products.
Get your feet checked at every visit with your primary care provider. See your podiatrist at least yearly for a complete foot exam.
Keep the blood flowing. Wiggle your toes for a few minutes several times throughout the day if possible. Do not do this in tight fitting shoes. Exercise, such as taking a walk, 10-20 minutes a day if possible. Choose feet-friendly activities like walking, riding a bike, or swimming. But always consult your doctor before beginning any exercise regimen.
Stop smoking. Smoking makes it harder for the body to regulate blood sugar levels and changes how your cells react to insulin. This can lead to unhealthy blood sugar levels. Smoking can also reduce blood flow to the feet by causing blood vessels to constrict. This may result in a delay of healing of any wounds you may already have on your feet.
Eat a sensible diet while limiting foods high in sugar, salt, and refined carbohydrates. Eat a healthy diet that’s high in fiber and nutrients, and low in calories. Focus on healthy low calorie and high fiber diet such as fruits, vegetables, lean proteins, whole grains, legumes, and low fat dairy products. Avoid less healthy carbohydrates, such as foods or drinks with saturated fats, sugars and sodium. Consult a nutritionist for more information on healthy food choices.
Monitor your blood sugar as indicated by your physician and keep a record of your results. You can use a continuous glucose monitor (CGM) to track your glucose levels throughout the day and night.
Take medicines as prescribed by your doctor and follow up regularly with your primary doctor and podiatrist.
Notify you doctor if you have:
- A cut, blister, or bruise on your foot that does not start to heal after a few days
- The wound or sore that gets infected. This may be seen as the skin on your foot that becomes red, warm, or painful
- A wound that is slow to heal
- A callus with dried blood inside of it which may indicate a wound under the callus
- A sore that turns black or smells bad
- Ingrown, thickened, or yellow toenails
- Dry or cracked skin on your feet
- Pain or swelling in you legs, feet, or ankles
Healing a Diabetic Foot Ulcer
conclusion
Diabetes can cause different types of problems with your feet. This usually happens because you have damaged nerves or blood vessels due to the long term effects of high blood sugars. Because you may lack feeling in your feet, small problems can go unnoticed and create serious complications.
Managing your blood sugar is crucial for avoiding foot problems. It is important to monitoring your glucose levels regularly, take your medications as prescribed, carefully planning meals, and going to your medical appointments.
There are steps you can take to prevent foot issues and complications. You should be sure to add your feet to your daily diabetes care. And don’t hesitate to reach out to your healthcare provider if you have any questions or concerns about the health of your feet.